Diagnosis
Consult to prevent pathology from worsening
Diagnosis basics
The ophthalmologist can use a questionnaire (often filled in by the patient in the waiting room) to assess the severity of symptoms. Repeated at each consultation, it is also useful for assessing the evolution of the disease over time and the effectiveness of treatments.
If symptoms suggest a dry eye condition, the ophthalmologist can use a variety of tests to assess tear quantity deficiency. The most classic, the Schirmer 1 test (without anaesthetic), involves placing a strip of filter paper on the lower eyelid. After 5 minutes, the wet zone is measured. Normal above 10 mm, dryness if < 10 mm, severe dryness if < 5 mm., secretion is considered normal. Below 15 mm, the tear film is insufficient.
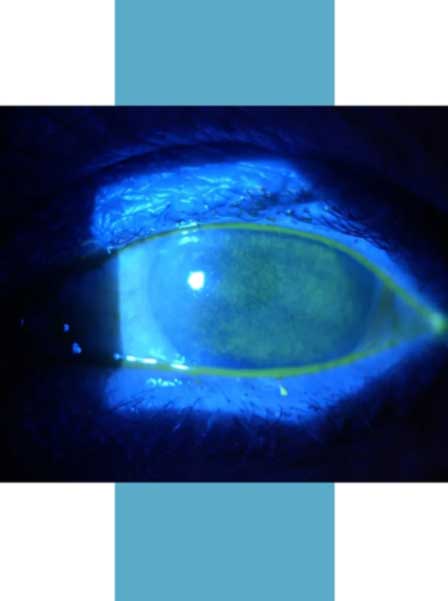
Using a slit lamp, the specialist performs a quick and simple examination to assess the tear film break-up time (BUT). After instilling a drop of fluorescein (dye), the practitioner observes how long this film covers the ocular surface evenly. A GOAL longer than 10 seconds is considered normal.
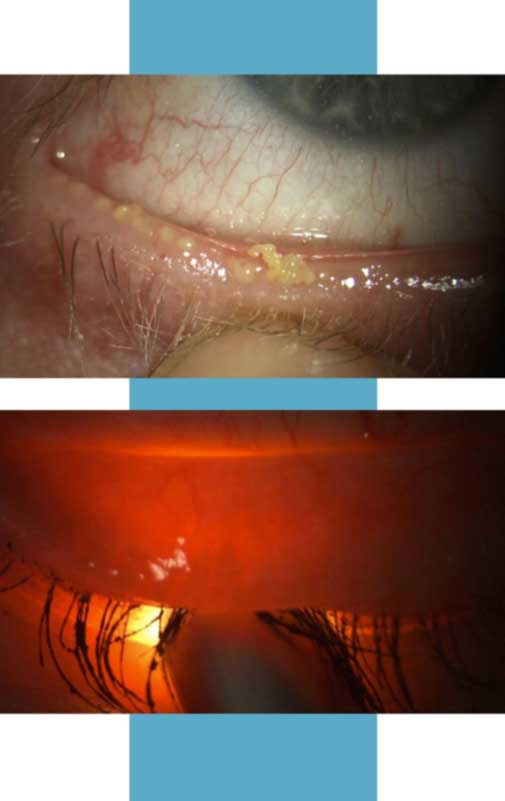
To assess the quality of the lipid film, the ophthalmologist examines the palpebral free edge, i.e. the transition zone between the skin and the conjunctiva of the eyelid. He looks for telangiectasia (a skin condition characterized by the dilation of small blood vessels) and/or meibum plugs in or on the orifices of the meibomian glands.
It also controls eyelashes, lacrimal meatus and the conjunctiva itself. He is also interested in meibum quality. It normally has the appearance of a light yellow fluid oil. If it’s dark yellow or white, or if its consistency is thick, granular or pasty, then it’s considered pathological.
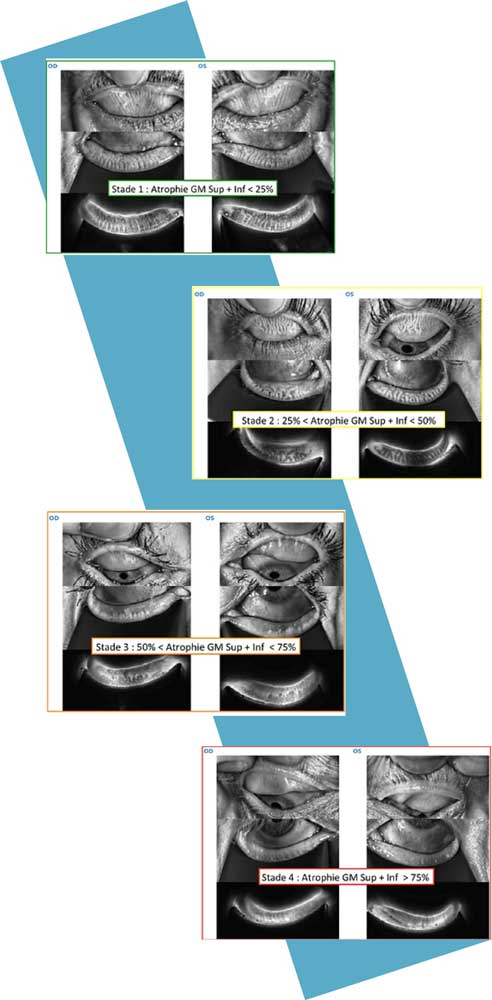
Finally, the ophthalmologist can assess the state of the Meibomian glands and their atrophy by everting the eyelids or using a retro-illuminator.
A final point of attention: inflammation. It may be obvious on examination, but this is not always the case. Tests can be used to refine the estimate. In just a few seconds, tears are sampled and a reagent is added.
The search for facial dermatological pathologies associated with dry eye (rosacea, dermatitis) completes the diagnosis.
A standard but thorough clinical examination will ensure that nothing is overlooked.
The meibograph:
an indispensable asset
Dry eye specialists have an additional tool at their disposal to perfect the diagnosis: the meibograph. This non-invasive instrument has been in use since 2010. An infrared camera and filter are used to illuminate the conjunctival surface of the eyelid. In this way, the ophthalmologist can establish a precise map of the state of the Meibomian glands and any atrophy. This mapping will enable us to monitor the evolution of the pathology. Finally, the meibograph can be used to refine the prognosis and help identify the causes of the symptoms experienced.
Given the importance of early detection and treatment of meibomian gland dysfunction, we recommend consulting a practitioner who uses a meibograph.